
Autoimmune Disease After Pregnancy
The postpartum period with a newborn is an exciting and joyful time. However, it can also be very exhausting and overwhelming!
A woman’s body goes through immense changes during pregnancy, and this is no different after delivery. It takes time for the body to return to “normal.” But even then, many women struggle with regaining optimal health in the years after pregnancy.
In our practice, we have noticed a pattern of autoimmune diseases developing in the year or two following pregnancy. This article will review autoimmune disease onset after pregnancy, why it’s more common, and what you can do to start feeling better.
What is Autoimmune Disease?
The immune system is designed to fight against unfriendly germs and bacteria. Typically, your immune system does a pretty good job at determining which cells are foreign (and dangerous) and which ones are your own cells.
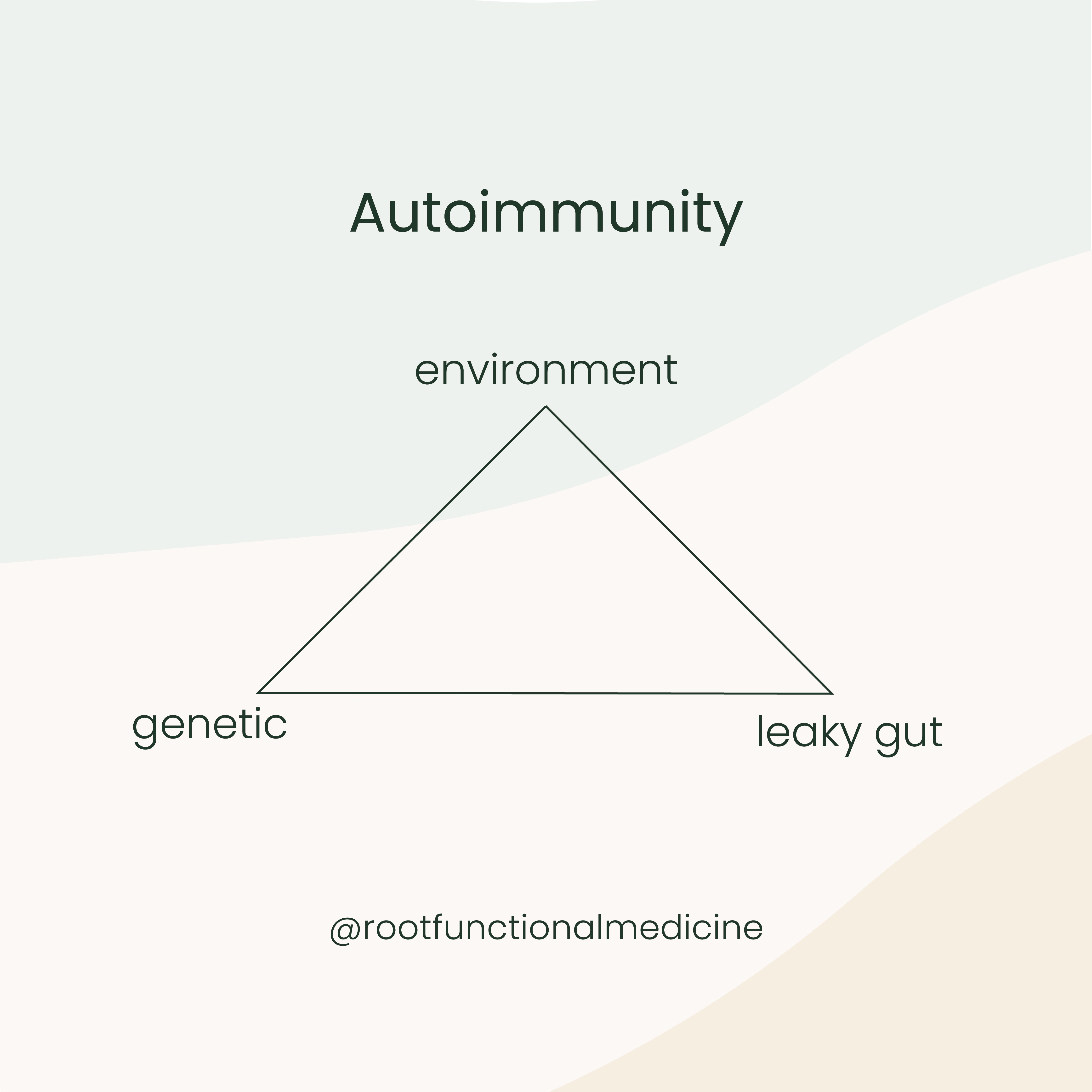
However, an autoimmune disease is a condition in which your immune system mistakenly attacks your own body. Autoimmune diseases are usually the result of a genetic predisposition, an environmental trigger, and changes in gut permeability (leaky gut).
The most common autoimmune diseases we see in our practice include:
- Hashimoto’s Thyroiditis
- Celiac Disease
- Rheumatoid arthritis
- Inflammatory Bowel Disease, like Crohn’s Disease or Ulcerative Colitis
We are most commonly seeing autoimmune thyroiditis (Hashimoto’s) in the postpartum period.
Why Autoimmune Disease After Pregnancy?
Researchers aren’t 100 percent certain why women experience more autoimmune disease in postpartum. However, there are many complex hormonal and immune-related shifts that occur during pregnancy. Fetal cells make their way into the mother’s circulation during pregnancy, and may remain in circulation long after delivery. Some researchers believe that this transfer of cells may be the underlying cause of higher autoimmune disease rates postpartum (1, 2).
Genetic Predisposition
If you have a family history of autoimmune disease, your risk of autoimmune disease after pregnancy may be higher. Studies also show that people with one autoimmune disease are also more likely to develop a second autoimmune condition (3).
Environmental Trigger
Environmental triggers are another suspected cause of autoimmune disease after pregnancy. Triggers can include emotional stress, like depression, anxiety, or feelings of overwhelm, or they may include physical stress, like sleep deprivation and postpartum nutrient deficiencies.
Leaky Gut
Many factors may lead to increased gut permeability postpartum.
Besides changes in the immune system, we may experience changes in the gut lining due to use of antibiotics, stress, lack of sleep, and nutrient deficiencies.
Our gut health bundle can be an excellent way to support gut health after pregnancy.
Gut Health Bundle
Our 3 most popular gut health supplements, bundled together for a 10% savings.
$182.00
Hashimoto’s and Pregnancy
While autoimmune Hashimoto’s thyroiditis can show up for the first time during pregnancy, the risk of onset is especially increased postpartum. In fact, up to 9 percent of all pregnant women develop hashimoto’s after pregnancy, which can present as either hyper- or hypothyroidism (4).
What is Hashimoto’s Thyroiditis?
Hashimoto’s thyroiditis is an autoimmune condition in which your immune system produces antibodies that attack your thyroid, a butterfly-shaped gland located at the base of the neck. Autoimmune thyroid disease affects eight times more women than men (1).
Symptoms of Hashimoto’s may include:
- Hair loss (more than what is normal postpartum)
- Depression or anxiety
- Extreme fatigue
- Decreased milk production in breastfeeding women
- Heart palpitations
- Dry skin
- Constipation
- Weight Gain
- Brain fog
Why is Hashimoto’s Often Missed?
A Hashimoto’s diagnosis after pregnancy can be missed because the related symptoms are often brushed off as normal postpartum stress, fatigue, and moodiness.
If your practitioner does run a thyroid screen, it will often only include one blood marker called Thyroid Stimulating Hormone (TSH). Unfortunately, testing only for TSH does not give us a full picture of how well the thyroid is functioning and does not test for thyroid antibodies (seen in Hashimoto’s).
Supporting your thyroid after pregnancy includes support for gut health, stress, a diet balanced for blood sugar, as well as replacing key nutrients to optimize thyroid function. Our Thyroid Support supplement contains these important nutrients and adaptogens for stress.
Autoimmune Disease and Pregnancy: What Can You Do?
Many of the environmental triggers for autoimmune diseases postpartum are unavoidable with a newborn. However, there are a few things you can do to help your body heal postpartum and start feeling better.
First of all, continue taking your prenatal vitamin postpartum. Pregnancy is physically taxing and often depletes women of many important nutrients. Meal trains are a great way to take the pressure off making delicious meals when baby first arrives. Furthermore, try to make self-care a higher priority as much as possible. Sleep whenever you can, delegate tasks, and take time to just rest. The laundry and cleaning can wait, mama! You deserve to take care of yourself. Don’t be afraid to ask for help.
If you feel like something is “off” since your pregnancy, do not be afraid to speak up. Ask your doctor if they can run a full thyroid panel (including TSH, T3, T4) with thyroid antibodies included to screen for Hashimoto’s after pregnancy.
Trying to navigate postpartum health issues and autoimmune conditions can be overwhelming and frustrating. At Root, we address the root cause of postpartum thyroid and/or autoimmune disorders. If you are looking for individualized support, we commonly work with people who have autoimmune conditions in our Root membership.
Get to the Root at Home
Curious about where you should start your functional medicine journey?
Take our Get to the Root Quiz so you can start working towards reversing disease and optimizing your health at the Root cause.
Take the Get to the Root Quiz
Related Articles

Best Vitamins for Hormone Balance
The best vitamins and nutrients for hormone balance include b-vitamins, vitamin D, omega-3s, inositol, magnesium, and NAC. These can be obtained via diet and supplementation.

5 Common Women's Health Problems That Can be Treated with Functional Medicine and Nutrition
Here at Root, we treat a variety of women’s health conditions with functional medicine and nutrition. Here is a list of 5 conditions we commonly work with: Hashimoto's thyroid, polycystic ovarian syndrome, irregular periods, irritable bowel syndrome, migraine


